Unique Immune Cells Present in Checkpoint Inhibitor-Induced Arthritis Patients, Discovered by Investigators
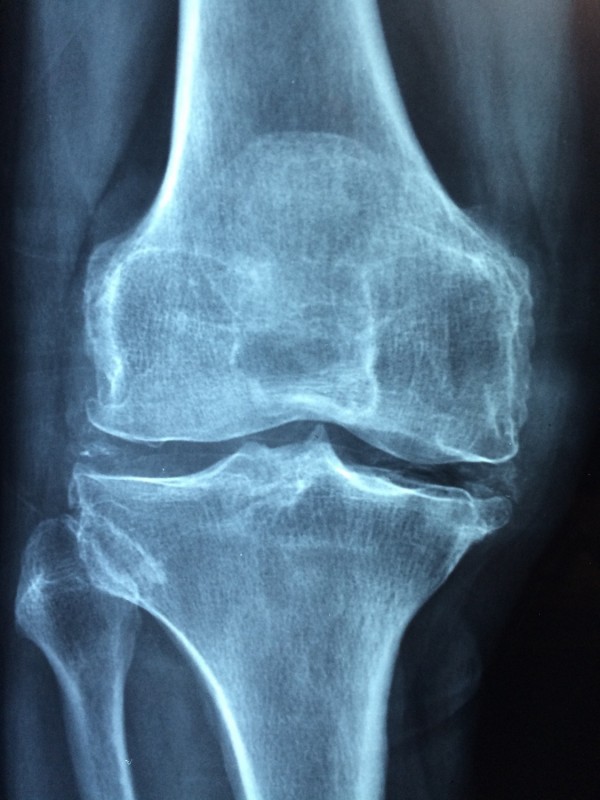
A study from the Hospital for Special Surgery (HSS) and Brigham and Women's Hospital researchers discovered that synovial fluid and blood of people having checkpoint inhibitor-induced arthritis is inhabited by a type of T-cells infrequently seen in people with other types of inflammatory arthritis. According to a release by HSS, the findings of the investigation are presented at the virtual American College of Rheumatology/Association of Rheumatology Professionals Annual Meeting.
According to the Hospital for Special Surgery, doctors began treating cancer patients with immunotherapy drugs named checkpoint inhibitors almost ten years ago, and they have detected that a subgroup of these patients experiences side effects that clinically resembles inflammatory arthritis. They added that these drugs naturally break the immune cells called T-cells, allowing them to attack cancer and sometimes lead to the attacking of healthy tissues such as joints. National Cancer Institute further said that when these checkpoints are blocked, T-cells can kill cancer cells better.
In the release, HSS' rheumatologist Karmela Kim Chan, MD said that although checkpoint inhibitor-induced arthritis resembles other forms of inflammatory arthritis, the result of their study suggests that they are different from each other. HSS added that checkpoint inhibitor-induced arthritis happens in about five percent of people using immunotherapy drugs as medication.
READ ALSO: Immunotherapy Combo Stops Rare, Stage 4 Sarcoma in Teenage Patient
Method
According to the release of HSS, the researchers of the study focused on the synovial fluid and blood from ten cancer patients who have experienced this side effect. They also analyzed blood and synovial fluid from eleven people with rheumatoid arthritis and nine people with spondylarthritis.
Result
The researchers explained the unique inhibitors of CD38 CD127- CD8 T-cells designation, meaning they have high levels of a marker called CD38 and did not show or express a marker called CD127. The researchers also mentioned that these T-cells are extended in the blood and joint fluid of people with checkpoint inhibitor-induced arthritis.
According to Dr. Chan in the release, they still do not know if the populace of the T-cells is triggering checkpoint inhibitor-induced arthritis or if it is a shared feature of a larger population of people being treated with checkpoint inhibitor medication. She added that the next step is to study the blood and synovial fluid of more patients that are being treated with these drugs and not limit their analysis only to those who are experiencing the side effects. She further said that researchers will eventually be able to concoct treatments that will target the T-cells that cause joint inflammation, which could be used to treat these side effects of immunotherapy.
ALSO READ: Scientists Test the Combination of Immunotherapies to Eliminate Solid Tumors
Immunotherapy and Joint Pain
Cancer.net defined immunotherapy as biologic therapy where it boosts the body's natural defenses in fighting cancer. They added that checkpoint inhibitors use substances made in the laboratory or by the body to improve, target, and restore immune system function. Cacer.net stressed that certain types of treatment slow the spread or attack cancer cells, making them easier for the immune system to eradicate. According to John Hopkins Medicine, a case report released in 2016 that 13 cancer patients taking the immunotherapy drugs ipilimumab and nivolumab may be at some higher risk of developing autoimmune joint and tissue diseases such as inflammatory arthritis.
READ NEXT: Treatment Booster for Metastatic Melanoma Discovered, Making Them Less Toxic
Check out more news and information on Immunotherapy on MD News Daily.
Nov 09, 2020 07:00 PM EST